The impact of high-cost medical and workers' compensation claims, both in-network and out-of-network -- is astounding. As the nation's payors, TPAs, self-insured employers and stop loss carriers face the challenges of managing these extraordinary expenses, they are also pressured to comply with ERISA and other regulations while ensuring care quality.
Here are some of the staggering facts: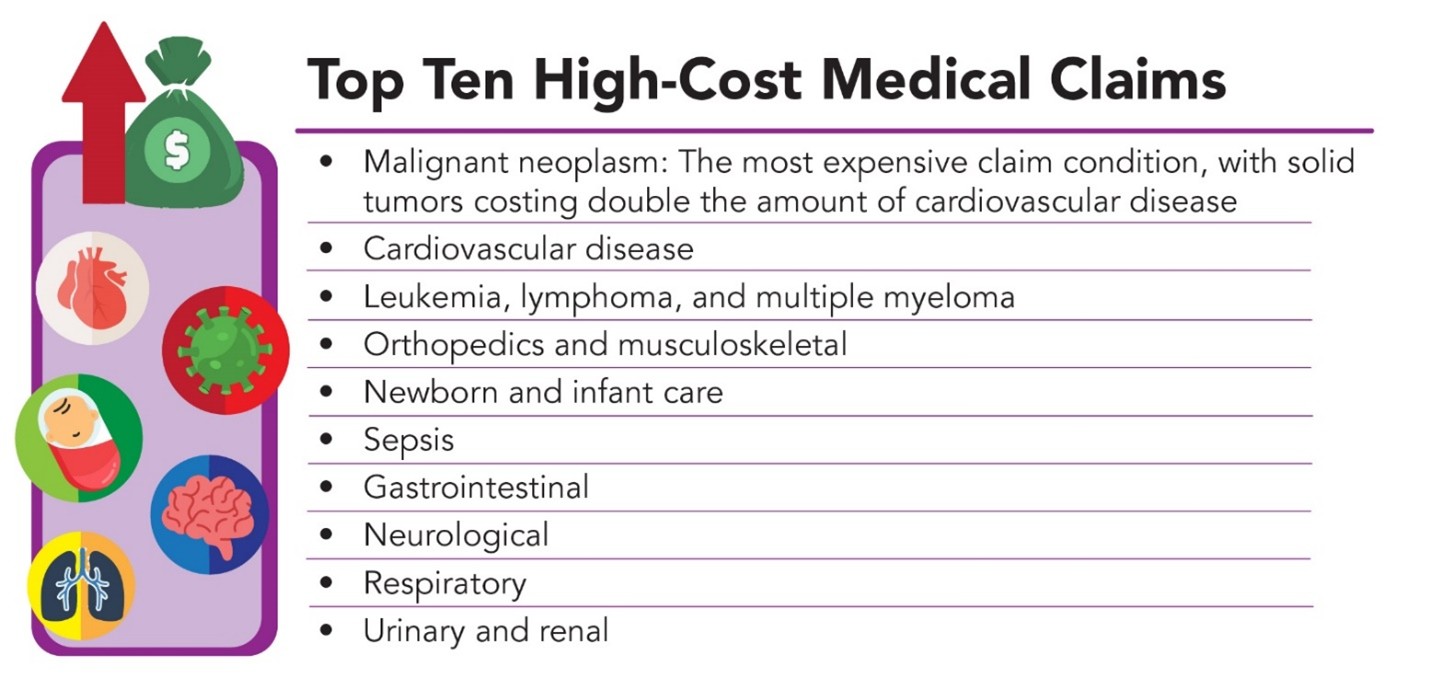
This is where H.H.C. Group steps in, offering unparalleled expertise and tailored solutions to help clients tackle even the most challenging claims.
H.H.C. Group specializes in reducing the financial burden of high-cost claims through a combination of expert claim negotiation powered by advanced technology and AI, independent review and repricing solutions. These services are designed to streamline the claims review process while ensuring fair and balanced outcomes for all stakeholders.
H.H.C.'s skilled negotiators work directly with providers to achieve cost savings, often reducing claim costs by as much as 90%. By leveraging deep industry knowledge and proven strategies, H.H.C. ensures fair pricing while maintaining provider relationships.
As a URAC-accredited Independent Review Organization (IRO), H.H.C. delivers unbiased evaluations of high-cost claims. This dual clinical and financial review process ensures:
Time-sensitive claims demand rapid action. H.H.C. completes most claim reviews and repricing within 5–7 days, empowering clients to make timely decisions and minimize administrative delays.
A 30-year-old female patient required a complex laparoscopic procedure to treat abnormal bleeding related to a rare anatomical condition. The provider billed $343,638.80—but within just three business days, H.H.C. Group negotiated the claim down to $68,000.00, achieving an 80.2% reduction ($275,638.80 in savings).
This outcome not only relieved significant financial pressure but also reinforced H.H.C. Group's ability to deliver fast, measurable savings—even in highly complex cases.
What sets H.H.C. Group apart is its client-centric approach and commitment to delivering customized solutions. Unlike competitors that rely heavily on automated systems, H.H.C. offers a personalized touch, tailoring strategies to the unique needs of each client.
Key differentiators include:As healthcare costs continue to rise, addressing high-cost claims will remain a priority for organizations striving to balance financial sustainability with quality outcomes. By partnering with H.H.C. Group, clients gain a trusted ally with the expertise and tools to tackle these challenges head-on.
Contact us to learn more about how H.H.C. Group can help your organization reduce healthcare costs and manage high-cost claims.